Since the healthcare world is moving towards establishing remote medical services as the norm, Remote Patient Monitoring (RPM) is becoming increasingly valuable and in high demand. What infused this approach is the COVID-19 outbreak, making RPM one of the most influential infection-control measures on a global scale. The benefits of RPM are more evident to physicians, healthcare professionals, hospitals, patients, and individuals since the technology is throwing them a lifeline to not only curb the 2019 Coronavirus (COVID-19) pandemic but managing chronic conditions as well.
The US Government & Medicare’s Crucial Steps to Support Curbing COVID-19
As COVID-19 continues to spread, the US government considers RPM technology as one of the safest and most effective methods for doctor-patient communication, since it provides healthcare follow-ups via phone, audio/video, text messaging, and email. The government also announced expanding Medicare telehealth coverage, allowing people to receive healthcare services from their doctors without having to commute to a healthcare facility. This ensures that Medicare beneficiaries can follow-up with their healthcare providers from their homes, avoiding being put at risk of getting infected with the virus or infecting others.
As reported by cms.gov, US Healthcare providers requested the following steps from the Coronavirus Aid, Relief, and Economic Security Act, or CARES Act:
- Expand the healthcare workforce by removing obstacles for physicians, nurses, and other clinicians to get hired from the local community or other states.
- Ensure that local hospitals and health systems can treat COVID-19 patients through temporary expansion sites (also known as the CMS Hospital Without Walls initiative).
- Increase access to remote medical care solutions for Medicare patients so they can get care from their physicians and other clinicians from the safety of their homes.
- Expand at-home and community-based testing to minimize transmission of COVID-19 among Medicare and Medicaid beneficiaries.
- Put patients over paperwork by giving providers, healthcare facilities, Medicare Advantage and Part D plans, and states temporary relief from many reporting and audit requirements so they can focus on patient care.
Why NOW is the Best Time for Physicians to Start Using RPM Technology!
-
Experiencing Better Health Outcomes
Improving the health outcomes of patients and treating them efficiently and effectively is the physicians’ ultimate goal. In this critical time, RPM helps healthcare providers with the early detection of any COVID-19 symptoms. The software technology helps them in monitoring and engaging with their patients and directing them to treatment and the infection-control procedures to be considered.
The real-time transmission of data helps educate and motivate patients to reshape their lifestyle and experience better clinical results. Furthermore, patients’ behavioral changes lead to improved care and quality outcomes with a positive impact on their overall health. Hence, we can fairly say that remote patient monitoring helps resolve critical challenges in care coordination.
-
Increasing The Practice’s Revenue
Due to the global pandemic, hospitals and healthcare organizations were beaten by a major loss of revenues. The integration of RPM technology into their systems as an infection-control measure turns out to be one of the most effective means of bridging the gap of the lost revenue caused by the COVID-19 outbreak. Other than being HIPAA-compliant, some of the invaluable features of RPM are seamless patient experience and enrollment, analyzable care plans, a comprehensive dashboard, 24/7 patient access portal, and the support for almost all devices.
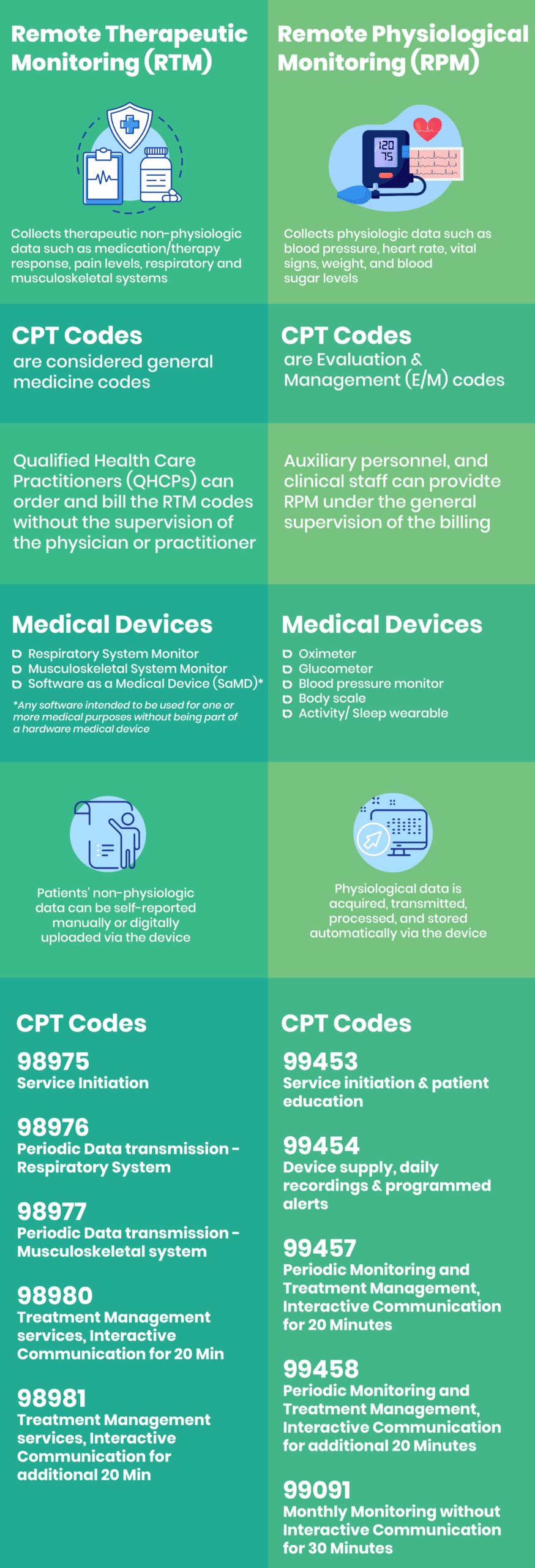
Moreover, RPM has Medicare reimbursement codes: CPT 99453 with $21 on-time payment for RPM setup and patients’ education, CPT 99454 with $69 monthly payment for RPM device supply, and CPT 99457 with $53 monthly payment for RPM periodic monitoring. When connecting the dots, you will realize that RPM offers services to help your practice generate even more revenue while providing your patients with better care.
-
Achieving Higher Efficiency with Maximum Support
Support takes two! Patients’ approval and support are crucial for the successful implementation of RPM programs. RPM software’s seamless integration into physicians’ workflows is among the proposed efforts to curb COVID-19, helping medical practitioners offer patients with the support and education needed to use RPM devices and technology.
Consequently, this effective doctor-patient collaboration to use RPM increases the efficiency of the medical treatments provided. Being senior-friendly is one of the main reasons why RPM technology is attractive. Also, having efficient, personalized care plans for every patient with secure two-way messaging gives both patients and doctors a safe method of communication with ultimate support.
-
Accessing Patients’ Data 24/7
RPM technology collects, tracks, and transmits patient health data from a patient’s home to a healthcare provider in a different location. To detect any early symptoms of COVID-19, patients need a device with RPM software to upload their vitals and health-related readings to, so their physicians can keep track of their overall health. Since country lockdowns are in-effect, individuals avoid going out of their home, especially to any medical facility with direct exposure to patients and medical staff.
Being able to access the data on the RPM’s comprehensive dashboard at any time of the day is the safe door to medical follow-ups until the crisis is over. The easy-to-use RPM software is designed to save time for both patients and physicians with 24/7 access to patients’ portals. The ease of accessibility to patients’ data and information attracts them to maintain updating their health readings and vital parameters periodically through the health trackers.
-
Reducing Face-To-Face Visits
With countrywide lockdowns taking place to impose social distancing and self-isolation, reducing, if not entirely hindering, face-to-face medical visits are a necessary step. RPM offers medical practices the ability to provide medical care to patients without risking coming into contact with infected individuals at healthcare facilities.
To execute the worldwide protocols and procedures of curbing the virus, reducing face-to-face interactions between patients, individuals, and healthcare practitioners are the main aim. They are all strongly encouraged to use RPM technology to continue their medical care plans without the risk of exposure.
Remote monitoring helps increase the work capability of physicians, providing treatment to more people at a time. As more healthcare providers open their businesses to emerging RPM technology, patients across the nation will attain better access to high-quality medical care right from their own homes. With or without COVID-19, RPM is not an option but rather a necessity, not only to cope with the worldwide procedures and measures but to shape a brighter future of healthcare and medical practices.