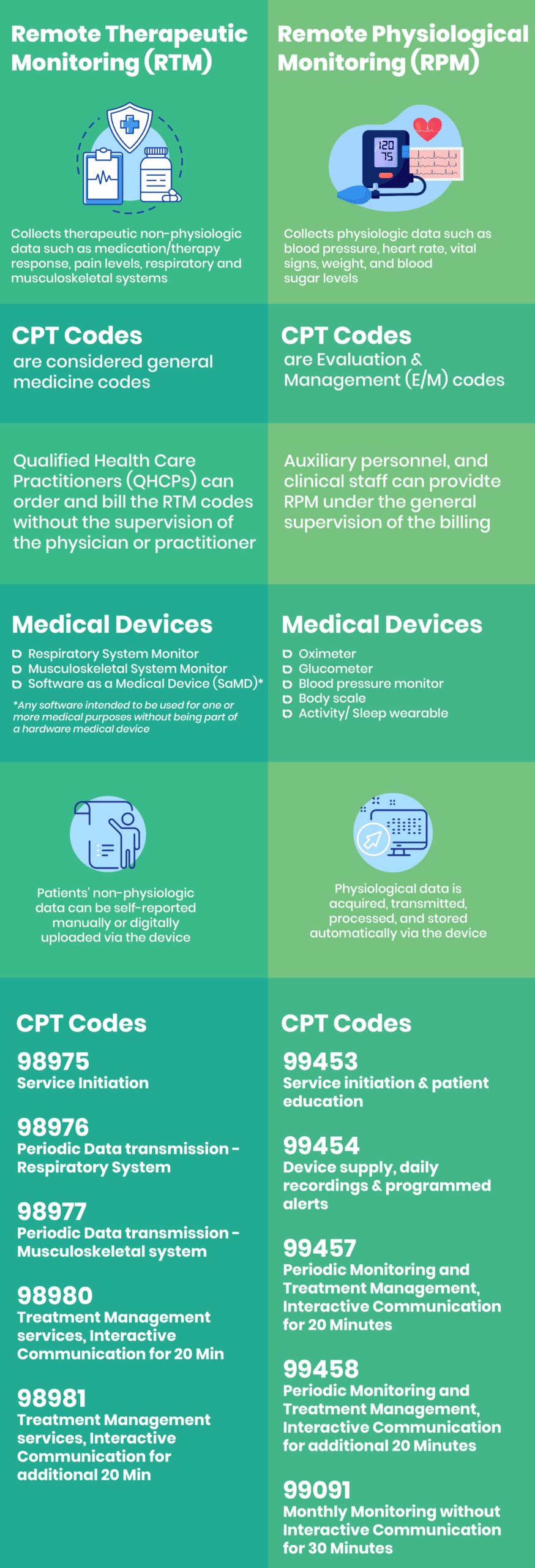
Continuing the trend of expanded Medicare reimbursement programs for remote monitoring, the Centers for Medicare and Medicaid Services (CMS) released five new Remote Therapeutic Monitoring (RTM) codes.
In the 2022 Final Rule, CMS emphasized its intent to maintain payment parity between the RPM and RTM treatment management codes. CMS also mirrored the RTM codes for initial setup and patient education and supply of medical devices to the corresponding RPM codes. CMS aligned the RPM and RTM codes to achieve the dual goals of extending the categories of patient data utilized to monitor treatment management services remotely, and augmenting the types of health practitioners who can order and bill for these services. This is a promising opportunity for practitioners and digital health companies alike, and most importantly, for patients.
We at TrueBlue MD understand that there are some typical questions that practitioners may have about RTM, and we’re here to answer them.
-
Which types of patient data can physicians monitor via the Remote Therapeutic Monitoring codes?
CMS discussed “therapy adherence” and “therapy response” concerning RTM, referring to monitoring health conditions where “non-physiologic data” is collected that’s related to musculoskeletal system status and respiratory system status.
Interpretation of “health conditions” is broad, and the focus on “musculoskeletal system status” and “respiratory system status” plays a significant role in limiting reimbursement for “device supply” to devices related exclusively to those two systems.
-
Which physicians’ taxonomies can order and bill for Remote Therapeutic Monitoring?
Qualified Health Care Practitioners (QHCPs) who are eligible to bill the general Medicine codes can order and bill for RTM services like physical therapists, occupational therapists, dietitians, and clinical psychologists.
These practitioners can order and bill the RTM codes without needing a physician, non-physician practitioner (NPP), or supervision requirements, expanding general use cases for RTM considerably.
-
Which devices are used for Remote Therapeutic Monitoring?
All devices used for RTM must meet the FDA’s definition of a medical device (as opposed to, for example, a general wellness device). Patients’ self-reported data is collected and transmitted via Software as a Medical Device in addition to standalone peripheral devices.
As finalized, the RTM treatment codes are not limited to musculoskeletal and respiratory systems health conditions. However, both “device supply” codes specifically refer to musculoskeletal monitoring and respiratory monitoring devices, leaving significantly fewer reimbursement opportunities for devices that do not fall into either category.
-
How are Remote Therapeutic Monitoring codes classified?
Unlike RPM codes, which are classified as Evaluation and Management (E/M) services, the RTM codes are considered general medicine codes that QHCPs can bill for without the supervision of a physician.
-
What are the minimum minutes required to bill for Remote Therapeutic Monitoring services?
CPT code 98980 is billed for a minimum of 20 minutes in 30 days dedicated to RTM treatment management of the patient, including at least one interactive communication (via phone or video) with the patient/caregiver during that month.
CPT code 98981 has the exact requirements as CPT code 98980, but it’s used for an extra 20 minutes per month as an add-on.
-
How many days must the device monitor the patient’s data?
The RTM device must monitor at least 16 days of data in 30 days to be able to bill for CPT codes 98976 and 98977
-
Will the patient be able to report their Remote Therapeutic Monitoring data manually?
Yes. In fact, CMS stated that self-reported/entered data is a part of the non-physiologic data included in the RTM codes. It can be self-reported by the patient or digitally reported via the device. According to CMS, self-reported RTM data via a smartphone app or online platform is classified as Software as a Medical Device (SaMD) and may qualify for reimbursement.
Remote monitoring won’t stop growing ins an area of significant technological potential over the coming years. Hospitals and providers use RPM, RTM, and other non-face-to-face technologies to seize these new revenue stream opportunities under CMS reimbursement programs. Practices must start offering remote monitoring technologies and services to develop patient population health, drive recurring revenue, and improve the patient care experience. Don’t you agree?